What is Micro-clotting?
Most people are familiar with the dangers linked to blood clots, but may not be aware of or understand the types of complications that can also develop due to micro-clots. Physical injuries and certain health issues may trigger blood vessel (vein) damage. If this occurs, cells in the bloodstream called platelets immediately begin to bind together at the site of damage to form a plug or clot on the blood vessel wall [1].
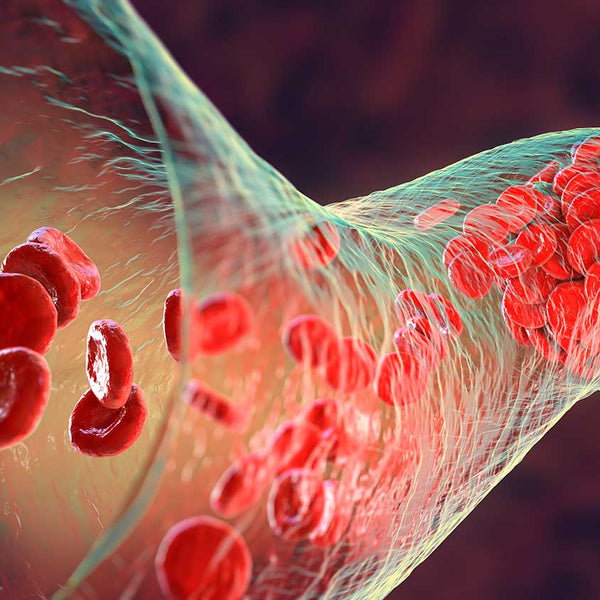
The platelets also interact with fibrin—a fiber-like protein that encourages blood clot formation by encasing platelets and other blood cells to create a clot. If this process takes place in a capillary—the smallest blood vessel in the body—it is known as a micro-clot.
Micro-clots are harder to detect than clots that form in veins (larger blood vessels) and are associated with two main problems: abnormal inflammatory levels and endothelial activation [1, 2]. Health problems and injuries often activate inflammatory responses that may involve the formation of a temporary micro-clot as cells work to heal the capillary wall. As the capillary begins to heal, the levels of a protein called plasmin begin to elevate. One of plasmin’s main functions is to dissolve the fibrin-based micro-clot [1]. Under unhealthy states (e.g., abnormal inflammation levels), micro-clots may resist breakdown by plasmin and contribute to another issue called endothelial activation [2].
Endothelial activation is a process by which blood-borne invaders and environmental pollutants cause endothelial cells that line blood vessels to undergo harmful changes that alter their function [2]. The functional changes lead to elevated white blood cell activity and movement into blood vessels. Heightened release of proteins and other molecules that worsen unhealthy inflammation levels also occurs. One of the harmful molecules is alpha 2-antiplasmin (α2AP), which causes micro-clots to resist plasmin breakdown. These processes gradually cause blood vessel damage that may become life-threatening [2].
References
- Pieters M, Wolberg AS. Fibrinogen and fibrin: An illustrated review. Res Pract Thromb Haemost. 2019;3(2):161-172.
- Deanfield JE, Halcox JP. Rabelink TJ. Endothelial function and dysfunction: Testing and clinical relevance. Circulation. 2007;115(10):1285-1295.
- Mazzone A, Catalani M, Costanzo M, et al. Evaluation of Serratia peptidase in acute or chronic inflammation of otorhinolaryngology pathology: A multicentre, double-blind, randomized trial versus placebo. J Int Med Res. 1990;18(5):379-388.
- Al-Khateeb TH, Nusair Y. Effect of the proteolytic enzyme serrapeptase on swelling, pain and trismus after surgical extraction of mandibular third molars. Int J Oral Maxillofac Surg. 2008;37(3): 264-268.
- Pais E, Alexy T, Holsworth RE Jr, Meise HJ. Effects of nattokinase, a pro-fibrinolytic enzyme, on red blood cell aggregation and whole blood viscosity. Clin Hemorheol Microcirc. 2006;35:139-142.
- Sumi H, Hamada H, Tsushima H, et al. A novel fibrinolytic enzyme (nattokinase) in the vegetable cheese natto: A typical and popular soybean food in the Japanese diet. Experientia. 1987;43(10):1110-1111.
- Ren NN, Chen HJ, Li Y, Mcgowan GW, Lin YG. [A clinical study on the effect of nattokinase on carotid artery atherosclerosis and hyperlipidaemia]. Zhonghua Yi Xue Za Zhi. 2017;97(26):2038-2042.